
If you’ve noticed your vision becoming blurry, more sensitive to light, or just not as sharp as it used to be, it might be easy to blame it on something like dry eyes or eye strain. But sometimes, there’s something deeper going on. One condition that often flies under the radar is keratoconus. It’s not very well known, but it can have a big impact on your eyesight if it goes undiagnosed. Let’s take a closer look at what keratoconus actually is, how it affects your eyes, and why it’s important to catch it early.
What is Keratoconus?
Keratoconus is a condition that affects the clear, front part of your eye called the cornea. Normally, your cornea is smooth and round, but with keratoconus, it gradually thins out and starts to bulge forward into a cone shape. This change in shape makes it harder for light to focus properly on the retina, which causes blurry vision and other problems. It usually starts during the teenage years or early adulthood and can slowly get worse over time.
What are the Symptoms of Keratoconus?
If you’re wondering whether you or someone else might have keratoconus, here are some common signs to look out for:
- Blurry or distorted vision: You may find it hard to see clearly, even with glasses.
- Increased sensitivity to light and glare: Bright lights might feel uncomfortable, especially while driving at night.
- Frequent changes in eyeglass prescription: Your vision may keep changing, and you might need new glasses more often than usual.
- Difficulty seeing at night: Low-light conditions can make it even harder to focus.
- Double vision or ghost images: You might see overlapping or shadowy images from one eye.
- Eye strain or discomfort: You may feel tired or sore eyes after reading or working on screens.
If any of these symptoms feel familiar or keep getting worse, it’s a good idea to get your eyes checked. Early diagnosis can help you manage the condition and prevent further vision problems.
Also Read: Keratoconus vs Astigmatism
What Are the Causes of Keratoconus?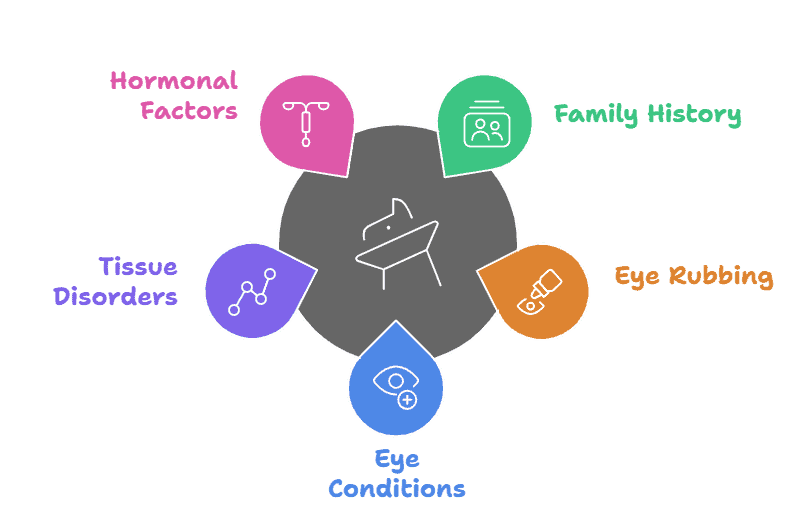
No one knows the exact cause of keratoconus. But over the years, doctors and researchers have found a few reasons that might explain why it happens. Both genetics and environmental triggers are believed to play a part. If you’re wondering what might lead to keratoconus, here are some possibilities to be aware of:
-
Family History
If someone in your family has keratoconus, your chances of developing it are higher. It’s often seen running through families, which suggests a genetic connection.
Also Read: The Role of Genetics on Your Eye Health
-
Frequent or Forceful Eye Rubbing
Rubbing your eyes too often or too hard can damage the cornea over time. People with allergies or constant eye irritation tend to do this without even noticing, and it may increase the risk of keratoconus.
-
Underlying Eye Conditions
Certain conditions, like chronic eye allergies, vernal keratoconjunctivitis, or atopic eye disease have been linked to keratoconus. These can cause long-term inflammation and weakening of the cornea.
-
Connective Tissue Disorders
Conditions like Down syndrome, Ehlers-Danlos syndrome, or Marfan syndrome are sometimes associated with keratoconus. These disorders affect the collagen and tissue strength in the body, including in the eyes.
-
Hormonal Factors
Some studies suggest that hormones might play a role in keratoconus progression, especially during puberty or pregnancy when hormonal changes are strong. This could explain why the condition often starts in teenage years.
How is Keratoconus Diagnosed?
Here’s how doctors usually diagnose Keratoconus:
-
Visual Acuity Test
The Visual Acuity test is a standard eye chart test that checks how clearly you can see. If your vision keeps changing or doesn’t improve with glasses, it could be a sign of something deeper, like keratoconus.
-
Slit Lamp Examination
During this exam, your eye doctor uses a special microscope with a bright light to get a close-up look at the front part of your eye. It helps them spot any thinning or bulging in your cornea.
-
Keratometry
This test measures the curve of your cornea. Since keratoconus causes the cornea to bulge, keratometry can help detect unusual shapes or changes early on.
-
Corneal Mapping (Topography and Tomography)
This is one of the most advanced and reliable ways to diagnose keratoconus. It creates a detailed 3D map of your cornea, showing its shape, thickness, and any irregularities that aren’t visible in standard tests.
What are the Treatment Options for Keratoconus?
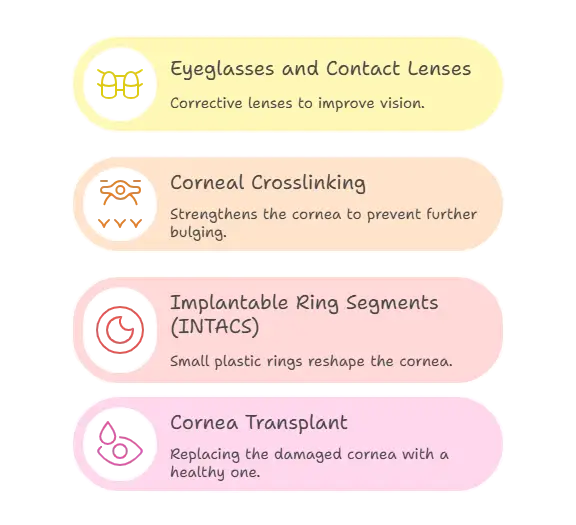
Once keratoconus is diagnosed, the next step is figuring out how to manage it. The treatment depends on how severe the condition is and how much it’s affecting your daily life. Here are the main options doctors usually recommend:
-
Eyeglasses and Contact Lenses
In the early stages, vision changes can be managed with regular glasses or soft contact lenses. As the condition progresses, rigid gas-permeable lenses or scleral lenses may be needed to improve focus and comfort.
-
Corneal Crosslinking
Corneal Crosslinking helps to slow down or stop the progression of keratoconus. It uses a special kind of UV light along with vitamin B2 drops to strengthen the cornea. It doesn’t reverse the condition, but it can keep it from getting worse.
-
Implantable Ring Segments (INTACS)
These are tiny curved pieces of plastic inserted into the cornea to reshape it and improve vision. They are a good option for people who can’t wear contact lenses and want to avoid a transplant.
-
Cornea Transplant
In advanced cases where the cornea becomes too thin or irregular, a transplant might be needed. The damaged cornea is replaced with a healthy donor cornea. It’s usually considered when other treatments no longer work.
Get Your Eyes Checked at InSight Vision Center
If you’re noticing blurry vision, increased sensitivity to light, or anything that feels off with your eyesight, it’s a good idea to get it checked early. At InSight Vision Center, our comprehensive eye exams go beyond a basic vision check. We use advanced diagnostic tools to look for conditions like keratoconus, which often goes unnoticed in its early stages.
Our expert team will take the time to understand your symptoms, examine your cornea’s shape and thickness, and walk you through your results clearly. If keratoconus is found, we’ll help you build a personalized treatment plan that fits your needs, whether that means specialty lenses, corneal crosslinking, or other treatments designed to protect your vision.
Getting checked early can make all the difference. Don’t wait until symptoms get worse.
Take the first step toward healthier eyes. Book your comprehensive eye exam at InSight Vision Center today
Frequently Asked Questions About Keratoconus

Dr. Azhar I. Salahuddin is an ophthalmologist and is fellowship-trained in cornea, external diseases, and refractive surgery. Dr. Salahuddin has been performing cataract surgery for over 19 years and specializes ocular reconstruction, corneal transplantation surgery as well as vision correction through a variety of intraocular lenses. Dr. Salahuddin is board-certified by the American Board of Ophthalmology and was trained at Boston University.

