Key Takeaways
- Keratoconus and dry eyes can feel very similar at first, with shared symptoms like blurry vision, irritation, and light sensitivity.
- Keratoconus is caused by thinning and bulging of the cornea, while dry eyes come from poor tear production or tear quality.
- Misdiagnosis is common, and using the wrong treatment can delay proper care and make symptoms worse.
- Both conditions can exist together, which makes a detailed eye exam the only reliable way to tell them apart.
- Early diagnosis and the right treatment plan are important to protect vision and improve comfort.
If your eyes constantly feel irritated, dry, or blurry, it’s easy to assume it’s just dry eye syndrome. But what if the discomfort is actually something else? Keratoconus, a progressive eye condition, can sometimes mimic the symptoms of dry eyes. This overlap often leads to confusion and even misdiagnosis. In this article, we’ll walk you through the differences between keratoconus and dry eyes, so you can understand what might really be behind the discomfort and when it’s time to dig a little deeper.
What is Keratoconus?
Keratoconus is an eye condition that affects the shape of your cornea, which is the clear front part of your eye. Instead of staying round, the cornea becomes thinner over time and starts to bulge outward, forming a cone-like shape. This change makes it harder for your eyes to focus properly, which can lead to blurry vision, light sensitivity, and trouble seeing clearly at night. It usually begins during the teenage years or early adulthood and may slowly get worse over time.
What are Dry Eyes?
Dry eyes happen when your eyes don’t make enough tears or the tears they do produce aren’t good enough to keep your eyes properly moist. This lack of moisture can make your eyes feel scratchy, irritated, or tired. You might notice a burning feeling, blurry vision, or even feel like something is stuck in your eye. If it’s not treated, dry eyes can sometimes lead to damage on the surface of the eye and make things worse over time.
What Are the Symptoms of Dry Eyes?
Here are some common signs you might notice when you are dealing with dry eyes:
- A stinging or burning feeling in your eyes, especially after reading or screen time.
- Redness or irritation that doesn’t go away easily.
- A gritty or scratchy feeling, like there’s sand stuck in your eye.
- Watery eyes, which sounds strange, but it’s your eyes overcompensating for dryness.
- Blurred vision or difficulty focusing, especially when blinking less.
- Sensitivity to light or wind makes it uncomfortable to be outside.
- Discomfort with contact lenses, making them feel dry or hard to wear.
These symptoms might be mild at first, but they can get worse over time if not addressed.
What Causes Dry Eyes?
Dry eyes can be triggered by many small things that build up over time. Here’s what could be causing it:
- Too much screen time without blinking often. This lowers tear production and dries out your eyes.
- Weather or air conditions, like dry wind, air conditioning, or heaters that pull moisture from your eyes.
- Aging, especially for people over 50. Tear production naturally slows down with age.
- Hormonal changes, particularly in women during pregnancy or menopause.
- Wearing contact lenses for too long, which can make your eyes feel dry and tired.
- Certain medications, such as antihistamines, antidepressants, or blood pressure drugs that reduce tear production.
- Health conditions, including diabetes, rheumatoid arthritis, or thyroid issues that affect eye moisture.
- Eye surgeries, like LASIK, which may temporarily reduce tear production.
If you think dry eyes are affecting your daily life, it’s worth talking to a doctor or eye specialist. With the right care, it can be managed easily.
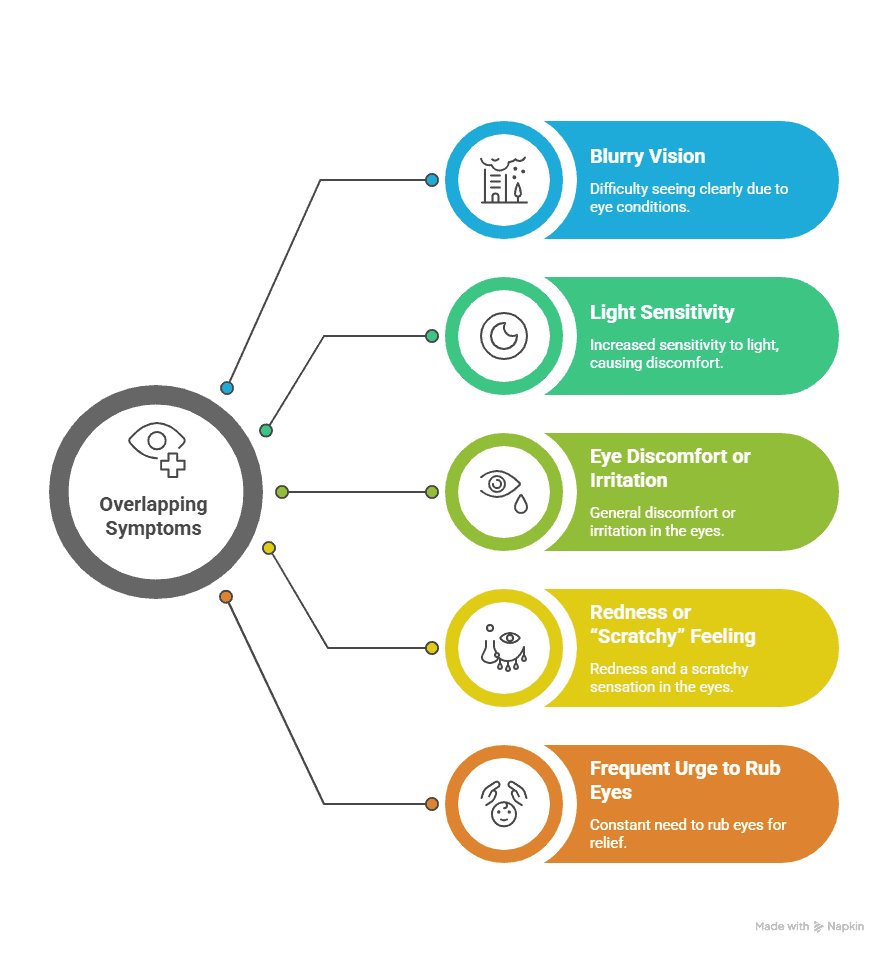
Overlapping Symptoms in Keratoconus and Dry Eyes: Why It’s Easy to Get Confused
Keratoconus and dry eyes might be completely different conditions, but the symptoms often feel very similar. If you’ve ever struggled to figure out which one you’re dealing with, you’re not alone. Here’s why things can get confusing:
-
Blurry Vision
Both conditions can leave your vision looking fuzzy or unclear. In keratoconus, it happens because the cornea changes shape. In dry eyes, it’s due to a lack of moisture that affects how light enters your eye. Either way, the result is the same, and things look blurred.
Also read: Cloudy Vision vs Blurry Vision: Causes and Differences
-
Light Sensitivity
Bright lights might start to feel too harsh or even painful. This happens in both conditions. Keratoconus changes the shape of your cornea, and dry eyes leave the surface irritated. In both cases, your eyes become more sensitive to light, especially during the day or while driving at night.
-
Eye Discomfort or Irritation
Whether it’s a dull ache or a burning feeling, discomfort is common with both. With dry eyes, the irritation usually comes from dryness and inflammation. In keratoconus, the discomfort may be from the eye working harder to focus or from contact lenses that don’t fit right. Either way, your eyes feel tired and uneasy.
-
Redness or “Scratchy” Feeling
Your eyes might look red and feel like they have something stuck in them. Dry eyes cause this because of reduced tear production, while keratoconus can lead to this due to ongoing stress on the eye. Either way, it’s irritating and uncomfortable.
-
Frequent Urge to Rub Eyes
Rubbing your eyes might seem like a quick fix when you’re uncomfortable, but it’s one of the worst things you can do, especially if you have keratoconus. Rubbing can worsen the condition by weakening the cornea. But when your eyes are dry, itchy, or irritated, it’s hard not to rub them. This is one of the most shared and most dangerous habits in both conditions.
Risks of Misdiagnosis in Keratoconus and Dry Eyes
Misdiagnosis in eye conditions like keratoconus and dry eyes isn’t uncommon, especially when the symptoms overlap in the early stages. If you’re experiencing frequent eye discomfort, blurry vision, or sensitivity to light, it can be hard to tell what’s really going on without a proper eye exam.
The problem is that both keratoconus and dry eyes can show similar early signs. Because of this, one condition may get mistaken for the other. When that happens, treatment is delayed or may not work the way it should. You might end up using the wrong eye drops or feel frustrated that your symptoms aren’t improving. Worse, if keratoconus goes untreated for too long, the condition can progress and lead to permanent changes in your vision.
When Can Both Conditions Coexist?
Sometimes, keratoconus and dry eye don’t just show up separately. They can exist at the same time. If you’ve been dealing with either, it’s important to understand how one can affect the other.
Keratoconus can make the tear film unstable, which can lead to more noticeable dry eye symptoms like irritation and blurry vision. On the other hand, if you have dry eyes and often rub them due to discomfort, that habit can actually increase your chances of developing or worsening keratoconus. It’s a cycle where one issue feeds into the other.
This is why getting a full eye exam is so important. Only a detailed check-up can reveal whether both conditions are present. The sooner they’re caught, the sooner your doctor can plan the right treatment to protect your vision and comfort. So if you’re noticing constant dryness, blurry vision, or changes in how your eyes feel, it’s a good idea to get them checked together.
Also Read: Keratoconus vs Astigmatism
Differences Between Keratoconus and Dry Eyes
| Aspect | Keratoconus | Dry Eyes |
|---|---|---|
| What It Is | A progressive eye condition where the cornea (the clear front part of the eye) becomes thin and bulges outward into a cone-like shape. | A condition where the eyes do not produce enough tears or the quality of tears is poor, leading to dryness and irritation. |
| Cause | Often linked to genetics, weak collagen in the cornea, oxidative stress, or frequent eye rubbing. | Can result from aging, excessive screen time, certain medications, environmental factors, or underlying health issues like autoimmune disorders. |
| Who It Affects | Usually starts in teenagers or young adults and may progress over time. | Can affect anyone but is more common in older adults, women, and those with prolonged screen exposure. |
| Symptoms | Blurred or distorted vision, increased sensitivity to light, frequent changes in glasses prescription, and difficulty seeing at night. | Burning, stinging, gritty sensation, redness, blurry vision that improves with blinking, and discomfort after reading or screen use. |
| Progression | Worsens gradually as the cornea continues to thin and change shape, leading to irregular astigmatism. | Symptoms may fluctuate daily and can worsen in dry or windy environments but are usually managed with proper care. |
| Impact on Vision | Distorts vision significantly due to the irregular shape of the cornea, often making glasses less useful. | Causes temporary blurriness, irritation, or watery eyes, but does not usually cause permanent corneal distortion. |
| Diagnosis | Confirmed through corneal topography, pachymetry (measuring corneal thickness), and slit-lamp examination. | Diagnosed by tear film tests like Schirmer’s test, tear breakup time, and clinical examination by an eye doctor. |
| Treatment Options | Glasses in early stages Special contact lenses (rigid, scleral, or hybrid lenses) Corneal cross-linking to stop progression Corneal transplant in severe cases |
Artificial tears and lubricating drops Medications to increase tear production Punctal plugs to reduce tear drainage Lifestyle changes such as reducing screen time and using humidifiers |
| Long-term Outlook | If untreated, it can severely affect vision and may require surgery. Early treatment helps stop progression. | Usually manageable with regular treatment. Rarely leads to serious vision loss but can affect quality of life. |
Diagnosing the Difference: What to Expect at Insight Vision Center
If you’re visiting Insight Vision Center for eye issues, here’s what you can expect during the diagnostic process, especially if the concern is keratoconus or dry eyes.
For keratoconus, the team usually starts with a corneal topography test. This gives a detailed map of the shape and curve of your cornea to detect any irregularities. Along with this, a slit lamp exam allows the doctor to closely examine the surface of your eye and spot any visible signs of thinning or bulging.
When it comes to dry eye, the approach is slightly different. You may undergo a Schirmer’s test, where a small strip of paper is placed under your lower eyelid to measure tear production. A tear film exam is also done to check the quality and stability of your tears.
Get a clear diagnosis for keratoconus or dry eyes at Insight Vision Center.?
The real clarity comes from how clinicians put all of this together. They listen to your eye-related symptoms, go through your medical and lifestyle history, and use specialized imaging tools to understand the root cause. Whether you’re struggling with distorted vision or constant dryness, the team combines all these pieces to pinpoint what’s really going on and guide you toward the right treatment.
Frequently Asked Questions (FAQs)

Dr. Azhar I. Salahuddin is an ophthalmologist and is fellowship-trained in cornea, external diseases, and refractive surgery. Dr. Salahuddin has been performing cataract surgery for over 19 years and specializes ocular reconstruction, corneal transplantation surgery as well as vision correction through a variety of intraocular lenses. Dr. Salahuddin is board-certified by the American Board of Ophthalmology and was trained at Boston University.